Blood Cell Formation and Hemoglobin Synthesis
Blood serves as a vital fluid in the human body, responsible for transporting oxygen, nutrients, and waste products. The formation of blood cells, particularly red blood cells (RBCs), and the synthesis of hemoglobin play crucial roles in maintaining homeostasis and ensuring that tissues receive adequate oxygen. This article provides an extensive overview of these processes, their underlying mechanisms, and their significance in health and disease.
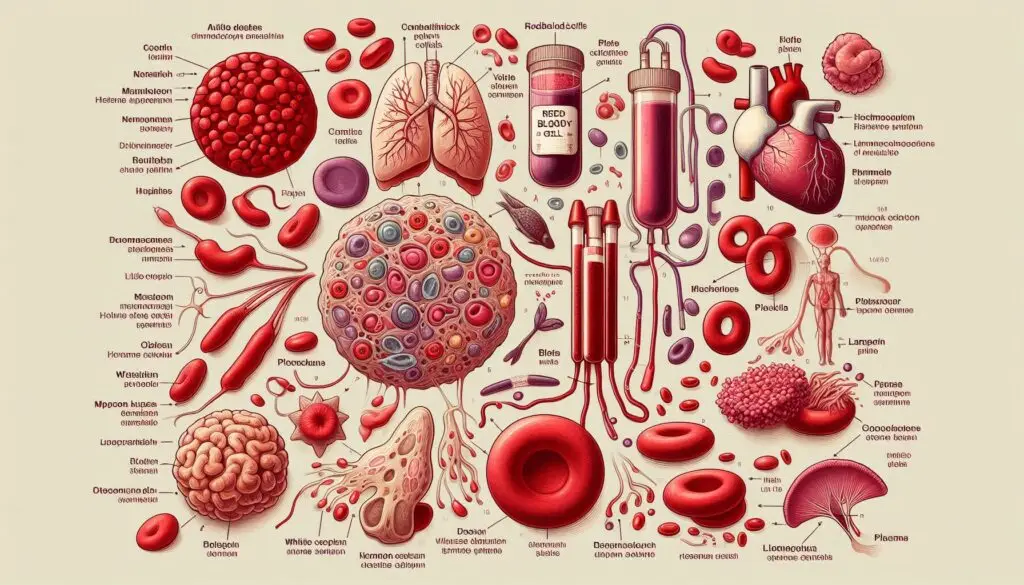
Introduction to Blood Cell Formation
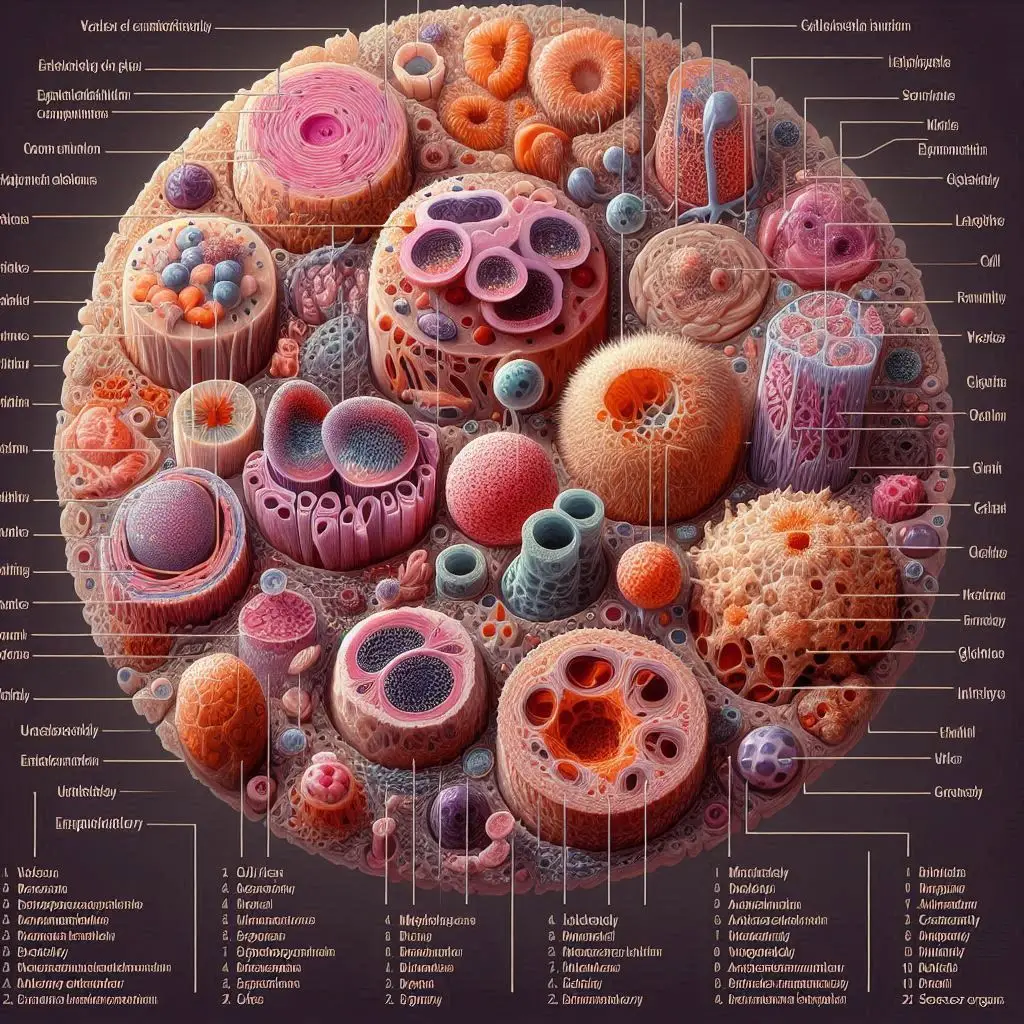
Blood cell formation, known as hematopoiesis, occurs primarily in the bone marrow. This complex process involves the differentiation of hematopoietic stem cells (HSCs) into various types of blood cells, including red blood cells, white blood cells, and platelets.
Hematopoietic Stem Cells
Hematopoietic stem cells are multipotent cells that can differentiate into all types of blood cells. These cells reside in the bone marrow and possess self-renewal capacity and differentiation potential. Consequently, they play a crucial role in maintaining the body’s blood supply.
Erythropoiesis: The Formation of Red Blood Cells
Erythropoiesis refers specifically to the process through which red blood cells are produced. This process can be divided into several stages.
Stages of Erythropoiesis
Proerythroblast Stage: The earliest precursor in erythropoiesis, proerythroblasts are large cells that undergo rapid division and differentiation. Erythroblast Stages: As proerythroblasts mature, they transition through several stages—basophilic erythroblasts, polychromatic erythroblasts, and orthochromatic erythroblasts. During these stages, hemoglobin synthesis begins. Reticulocyte Stage: After losing their nuclei, the cells become reticulocytes, which are released into the bloodstream. Here, they continue to synthesize hemoglobin before maturing into erythrocytes. Mature Erythrocytes: Fully mature red blood cells lack nuclei and organelles, allowing for maximum space for hemoglobin, which is essential for oxygen transport.
Hemoglobin Synthesis
Hemoglobin functions as a complex protein that plays a critical role in oxygen transport. It consists of globin chains and heme groups, and its synthesis intricately links to erythropoiesis.
Heme Synthesis
Heme synthesis occurs in the mitochondria and cytosol of erythrocyte precursors. The process begins with the condensation of succinyl-CoA and glycine to form 5-aminolevulinic acid. Subsequently, this compound undergoes several transformations to produce heme.
Globin Synthesis
Globin chains synthesize in the cytosol. In adults, hemoglobin typically consists of two alpha and two beta chains (HbA), while fetal hemoglobin (HbF) contains two alpha and two gamma chains. Researchers tightly regulate the synthesis of globin, which occurs concurrently with heme synthesis.
The Chemistry of Hemoglobin
Hemoglobin functions as an oxygen carrier, binding oxygen in the lungs and releasing it in tissues. The heme group contains iron, which is essential for its oxygen-binding capacity.
Oxygen Binding and Release
Hemoglobin exists in two states: the relaxed (R) state, which has a high affinity for oxygen, and the tense (T) state, which has a lower affinity. Factors such as pH, carbon dioxide levels, and 2,3-bisphosphoglycerate concentration in the blood influence the transition between these states.
Regulation of Erythropoiesis
Erythropoiesis undergoes regulation by various factors, including erythropoietin (EPO), a hormone produced by the kidneys in response to low oxygen levels. EPO stimulates the production of red blood cells by promoting the survival and proliferation of erythroid progenitor cells.
Clinical Significance of Blood Cell Formation and Hemoglobin Synthesis
Understanding blood cell formation and hemoglobin synthesis proves crucial for diagnosing and treating various hematological disorders, such as anemia, polycythemia, and sickle cell disease.
Anemia
Anemia occurs when a deficiency in red blood cells or hemoglobin leads to reduced oxygen transport. Various causes contribute to anemia, including nutritional deficiencies, bone marrow disorders, or chronic diseases.
Polycythemia
Polycythemia refers to an increase in red blood cell mass, which can lead to increased blood viscosity and complications such as thrombosis. This condition can be primary (due to intrinsic bone marrow disorders) or secondary (due to external factors like chronic hypoxia).
Sickle Cell Disease
Sickle cell disease represents a genetic disorder that affects hemoglobin structure, leading to the formation of rigid, sickle-shaped red blood cells. This condition can cause pain, anemia, and an increased risk of infections.
Advances in Blood Cell Manufacturing
Recent advances in biotechnology have led to new methods for producing red blood cells in vitro, using stem cells and bioreactor systems. These innovations hold promise for addressing blood shortages and improving transfusion medicine.
Stem Cell-Derived RBCs
Researchers actively explore ways to improve the efficiency of generating red blood cells from stem cells, including embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs). These advancements may enhance our ability to produce blood cells on demand.
3D Culture Systems
3D culture systems mimic the bone marrow niche and enhance the production of functional red blood cells by providing a conducive environment for cell growth and differentiation. This technology represents a significant step forward in regenerative medicine.
Conclusion
In summary, blood cell formation and hemoglobin synthesis represent fundamental biological processes that ensure the proper functioning of the human body. Advances in our understanding of these processes have significant implications for medical science, particularly in the fields of hematology and regenerative medicine.
For more pearls of Vets Wisdom:

Responses